The Future is Now
Since our founding in 1853, Sheppard Pratt has been transforming care and leading the way, creating a mental healthcare continuum that advances the field in modern, comprehensive, and accessible care and treatments. We have always been the place people turn to for behavioral health solutions, offering proven best practices that others look to for hope and healing. In the past few years, the need for behavioral healthcare has increased at a rapid pace. Nearly half of Americans will meet the criteria for a diagnosable mental health condition in their lifetimes, yet 55% of adults with a mental illness receive no treatment, according to Mental Health America. And the numbers confirm a downward trend for our youth as well, with suicide remaining a leading cause of death, and 60% of youth with major depression not receiving mental health treatment at all. With an eye toward the future, we’ve developed innovative solutions while expanding access to care to best serve the needs of our communities and every person who walks through our doors.
Today, we are in the midst of a mental health crisis, and the life-changing care Sheppard Pratt provides is needed now more than ever. The future we have been building toward is now.
This year’s annual report spotlights our vision to meet today’s demands. Sheppard Pratt is a nationally recognized leader. People from near and far trust us because the experts who are part of our team are the very people who are revolutionizing mental healthcare practices and solutions. The treatment options we offer are cutting edge and research based. We have built facilities, programs, and partnerships so that we can say “yes” to each person who walks through our doors and needs help. A new children’s hospital to tackle youth mental health, new “front doors to care,” technology that improves patient care, and partnerships that span the country are part of that future. That bold vision has defined— and continues to define—Sheppard Pratt. Our continuum of care is unlike any other.
And while the future is now, Sheppard Pratt will never stop growing and evolving. We stand ready to reimagine the future as we go—leading from the front, ready, and able to serve.
A Message From Our Board Chair and President
Dear Friends and Colleagues,
Sheppard Pratt was founded on Moses Sheppard’s life-changing directive to compassionately serve those with mental illness, and that vision has propelled our journey forward. It has driven us to create programs and services that are constantly evolving to meet the changing needs of our communities and the people we serve.
Our nation, our world, is at a precipice. The mental health crisis is here. The foundation we built in 1853 and have been building on ever since is needed now, more than ever. The key to our longevity has always been the ability to adapt and change. With the knowledge that our services are in great demand, we are taking bold steps, fueled by a bold vision. We are meeting those demands head on as the future is now.
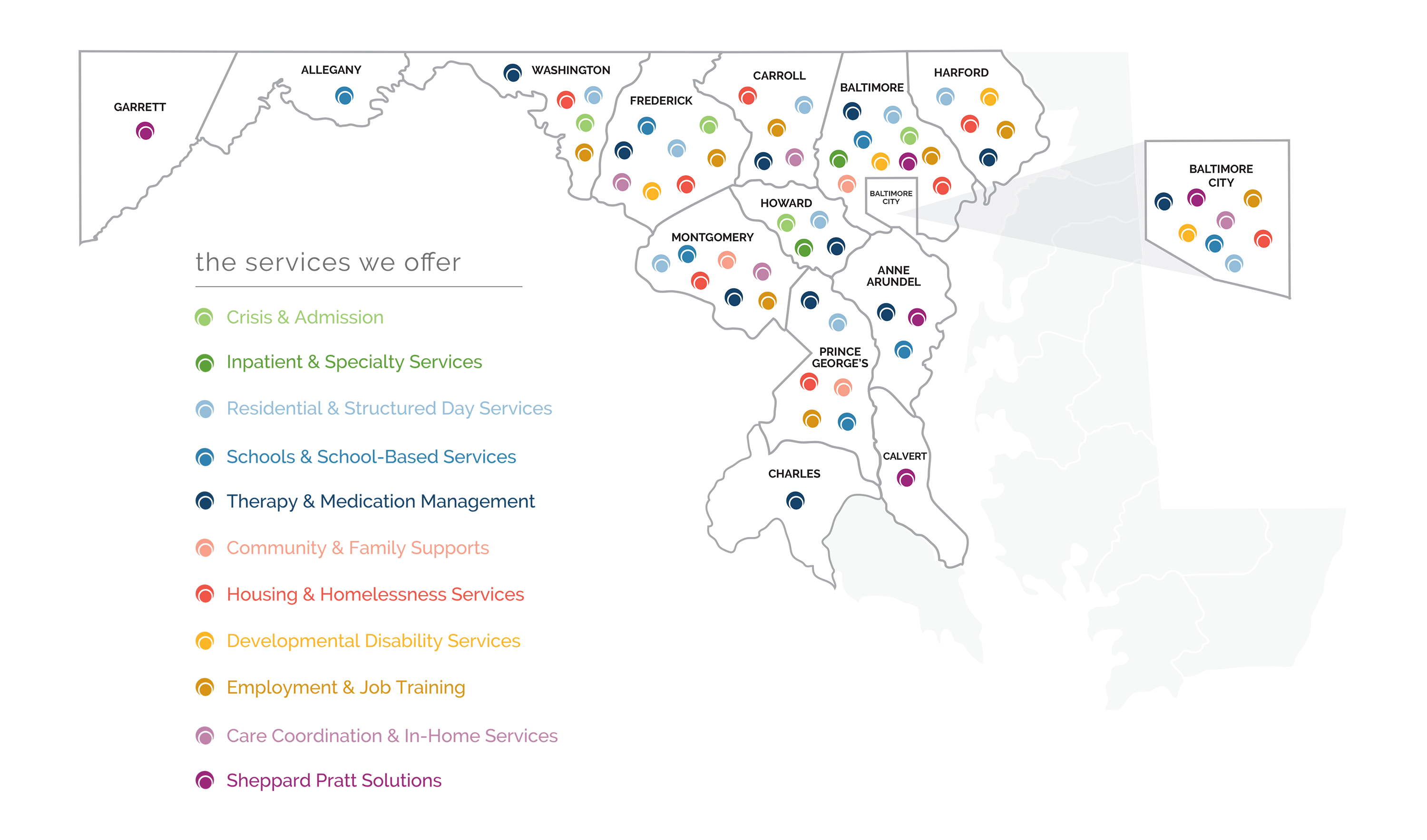
We serve nearly 80,000 individuals in more than 160 programs in Maryland and through our partnerships with hospitals and health systems across the country. We offer and support care and services that treat the whole person, from inpatient and outpatient treatment to rehabilitation services, housing, education, job training, and more.
Our mission has always been about helping people when they need it most. And in this critical moment, our path has never been more clear.
In this year’s report, you will learn how the youth mental health crisis has led directly to the bold vision we are bringing to life today to create the premier children’s mental health hospital in the nation—a vision that requires the support of all of us to make a difference. You will read about our “front door” to care, and how we are creating access in many ways to reach people where they are, especially those in crisis. You’ll see how our technology and continuous improvement processes are advancing patient care and outcomes. You’ll also learn how we are creating unique and innovative community partnerships that broaden our continuum of care. And you’ll dive deeper into the expansion of Sheppard Pratt Solutions, our consulting and management division, to learn why hospitals and health systems nationwide are partnering with us to make mental healthcare more accessible to meet the demands of their communities.
We continue to evolve and grow our programs and services with what we know people need today as well as what they will need tomorrow. The future is now, but our work continues. Join us.
Sincerely,
Josh Kakel, Chair, Sheppard Pratt Board of Trustees
Harsh K. Trivedi, MD, MBA, President and CEO, Sheppard Pratt
Eye to the Future
Delivering on our promise to develop innovative solutions while expanding access to care that best serves the needs of our communities.
Sheppard Pratt's Impact
Largest private, nonprofit provider of psychiatric services nationwide
Largest provider of nonpublic special education schools and programs in Maryland
Serving patients from 39 states & 15 countries
More than 380 sites of service
5,000 employees working for patient care every day
Consistently recognized as a top national psychiatric hospital
More than 160 programs throughout Maryland
Bringing a Bold Vision Forward for Today's Youth
Prior to the pandemic, young people were suffering, and the need for mental health support and services was substantial. In 2019, the Centers for Disease Control and Prevention reported that 5.8 million children across America were suffering from anxiety. Research from the National Center for Health Statistics demonstrated an alarming 57% increase in suicide rates between 2007 and 2018 for young people between the ages of 10 and 24.
Then, in 2020, the COVID-19 global pandemic began.
As the world shut down, the youth mental health crisis in America was exacerbated even further. Kids accustomed to busy lifestyles full of school, sports, friendships, family engagements, and social commitments faced changes that were once unimaginable. Their sports games and competitive seasons, music and dance recitals, and many other activities were canceled. Birthday parties, school dances, graduations, vacations, and holiday celebrations were all removed from the calendar. Uncertainty and disappointment dominated the ways kids felt. A greater reliance on social media and virtual connectivity left many feeling more isolated than ever. Today’s youth are in crisis.
“Each day I am contacted by a parent who needs our help,” said Harsh K. Trivedi, MD, MBA, president and chief executive officer of Sheppard Pratt. “This alarming concern is the drumbeat of how many calls are coming in and how much need there is. These anecdotes combined with the data of how many kids have thought about or attempted suicide, who are struggling to make it to tomorrow, this is the pandemic that we have failed to acknowledge as a community, society, and nation.”
The vision to transform youth mental health starts with bringing about changes that impact kids in this moment, expand much needed access, and meaningfully advance care and outcomes.
“As much as we talk about solutions, we need swiftness of action and boldness of resolution, as well as building solutions that impact people today,” said Dr. Trivedi. “This is the part of the conversation where Sheppard Pratt is uniquely different. We already provide the most comprehensive set of youth mental health services, with the greatest ability to quickly scale what we do to have population-level impact. This is something few across the nation can deliver upon.”
Under Dr. Trivedi’s leadership, there has been an unwavering commitment to addressing the youth mental health crisis. Sheppard Pratt already provides nearly 120 inpatient child and adolescent beds, and offers dedicated programs for anxiety, obsessive-compulsive disorder (OCD), eating disorders, and autism. It runs 11 special education schools, accommodates 50 children and adolescents through its partial hospital programs, has school-based programs embedded in more than 200 public schools, and outpatient and support programs across the state.
And now that commitment takes another step forward with a bold vision to build the premier children’s mental health hospital in the nation, dedicated to caring for children who are diagnosed with all types of emotional, behavioral, and mental health conditions— from anxiety and depression to autism, attention deficit/ hyperactivity disorder, eating disorders, mood and personality disorders, trauma and stress-related disorders, and substance use issues. The vision is to create a home, a trusted place families can turn to, that offers comprehensive treatment programs to address the specialized needs of every child all in one place. This beacon of hope will be the place for national experts and multidisciplinary teams of clinicians to convene, to find solutions, and to scale effective interventions. It will be the place to launch incredible initiatives for care today as well as build solutions and services that will impact a generation of youth. Children and their families will benefit from the expertise of Sheppard Pratt’s youth mental health specialists, the availability of the most advanced treatment options, individualized treatment plans, and the innovation that stems from research-based care protocols. This best-in-class hospital will serve as a national model for youth mental healthcare and be a premier clinical and research center to serve the residents of the state and the region.
“We have the capacity, the knowledge, the know-how, and the experts to be the national center to lead across all fronts in a way no one else in the nation can. Our vision is to create evidence- based care models, ensuring that they move the needle, and then share those best practices with communities across the nation that are committed to doing what’s best for our youth,” said Dr. Trivedi.
The children’s hospital will become the focus of activity across all programs and services. There are several key foundational elements that are part of the campaign to transform youth mental health and help each child live out their best tomorrow. Building upon the world-class programs on its flagship campus, Sheppard Pratt will support the growth of programs and services with an immediate impact. It will build onto existing teams to attract the nation’s leading child and adolescent clinicians, researchers, and educators to harness innovation and advance care outcomes. With a deep commitment to investing in its workforce, Sheppard Pratt will expand training across all disciplines—with a focus on communities of color—to shrink the provider gap and ensure all youth have timely access to care. Sheppard Pratt will also accelerate research from discovery to standard of care so that its world-class investigators can change lives daily by identifying new and effective ways to treat some of the most common youth mental health issues. Lastly, Sheppard Pratt will use its expertise to help change public perception and policies to make it easier for people to ask for help and to have mechanisms to provide sustainable mental health services across the nation. Through increased partnerships, education, and training, Sheppard Pratt will continue to lead the way and mobilize efforts to ensure policymakers prioritize funding for mental health and develop policies that bring hope and possibility to people’s lives.
The youth mental health crisis is a pandemic in and of itself and is one that needs to be acknowledged and managed now. The national statistics, coupled with Sheppard Pratt’s unprecedented pediatric patient volumes, underscore why a commitment to reimagining the process of care for children is so critically important. Sheppard Pratt has always been the place people turn to when their child isn’t getting better. Providers across the country have referred children to Sheppard Pratt when treatments have failed elsewhere. With the future opening of its premier children’s hospital, Sheppard Pratt will offer youth and families a place that propels care forward, impacting and improving lives in the shortest time possible.
“The earlier we can intervene and get a child the care they need, the greater our impact can be, and the better off our kids will be for years to come,” said Dr. Trivedi. “The services we provide can change the entire trajectory of a child’s future. No child should have to wait, and it will take all of us working together with a bold vision to make a difference. The future of our youth is at stake. And that future starts now.”
The earlier we can intervene and get a child the care they need, the greater our impact can be, and the better off our kids will be for years to come.
Creating Solutions for Healthcare Systems Across the Country
Wake County is the fastest growing county in North Carolina, and one of the fastest growing in the nation. A burgeoning area, but like many communities, behavioral health resources have been too limited to serve the growing demand.
“We have behavioral health capabilities in the emergency department and see more than 40,000 patients each year for behavioral health needs. In a time of growing need, we thought it was our duty to step up and provide critical inpatient behavioral health services for our community. To do this most effectively, we needed to secure a great partner to go on this behavioral health journey with us,” said Rick Shrum, MHA, MBA, vice president and chief strategy officer at WakeMed Health & Hospitals based in Raleigh, North Carolina.
From coast to coast, hospitals and healthcare systems of all sizes are feeling increased pressure to best serve their communities. For many, the need to launch or expand behavioral health services is a key strategic priority, and one that begs many questions: What scope of services should be integrated in order to meet the needs of our patients? What can we do to make those services convenient and accessible for all? How do we minimize or eliminate barriers to care? And, how can we operationalize changes or additions to our behavioral healthcare service line, in ways that best meet the needs of the community?
For more than 50 hospitals and healthcare systems located in 27 states across the country, including WakeMed, the answers have been found in partnership with Sheppard Pratt Solutions. These consulting, management, and development services of Sheppard Pratt are designed to help healthcare organizations nationwide establish and improve delivery of hospital- and community-based behavioral health services.
“In general, healthcare systems are challenged as they recover from the pandemic, and at the same time, there is a lot of pressure to build or grow behavioral healthcare services based on current and projected patient needs,” said Stephen Merz, FACHE, chief operating officer of Sheppard Pratt Solutions. “Hospital leaders are committed to creating new settings of care that are tailored to what their patients need, but many require guidance on how to plan and operationalize them. Solutions paves the way for hospitals and health systems, bringing to bear Sheppard Pratt’s 170 years of experience and expertise, and shedding light on what can otherwise be a difficult-to-navigate path.”
Sheppard Pratt’s reputation as a nationally recognized, evidence-based mental healthcare organization with renowned clinical experts, and the trust that comes with that, is the reason Solutions has grown rapidly since its launch in October 2021. Some healthcare systems have forged consultation agreements with Sheppard Pratt Solutions, seeking strategic guidance on what to do regarding current clinical care gaps or operational challenges. Others have established management agreements, which engage Sheppard Pratt resources and experts to manage existing behavioral healthcare services or develop new ones.
Behavioral health has long been part of WakeMed’s services, and the tremendous demand led to formalizing a growth plan. Pre-pandemic, WakeMed saw about 40,000 people annually with substance use or behavioral health needs, but that number rose 30% at the height of the COVID-19 pandemic. Today, leaders at WakeMed and experts from Sheppard Pratt Solutions are pursuing a bold vision that will transform the delivery of mental healthcare services in the region. Plans are underway for Sheppard Pratt Solutions to help develop and ultimately manage the day-to-day operations of WakeMed’s150-bed mental health and well-being inpatient hospital.
“We have a lot to think through operationally and also want to account for community use and patient accessibility as we design and construct our new building,” said Shrum. “Our partnership with Sheppard Pratt Solutions will help us reach decisions about how to optimize our mental health and well-being service line and shorten the time it takes for us to become a top 10 behavioral health provider.”
In a time of growing need, we thought it was our duty to step up and provide critical inpatient behavioral health services for our community. To do this most effectively, we needed to secure a great partner to go on this behavioral health journey with us.
The skills and expertise of Solutions are impacting communities large and small across the nation.
St. Mary’s Health System located in Lewiston, Maine, a member of Covenant Health, began its relationship with Sheppard Pratt Solutions in 2022 for consulting work before launching a management agreement in 2023. One of the oldest hospitals in operation in the state of Maine, it’s known for its vast portfolio of behavioral health services. Coming out of the COVID-19 pandemic, hospital leaders at St. Mary’s, like many hospitals and health systems across the country, were forced to reduce services, including their behavioral health services. One of just two hospitals in Lewiston, St. Mary’s provides the majority of behavioral health services. Understanding its importance in the community and the increased rate of substance use and other behavioral health needs, the board made the strategic decision to grow behavioral health services.
St. Mary’s partnered with Solutions to achieve key goals including: to develop a comprehensive vision to reestablish a full continuum of behavioral healthcare services, to put systems in place to enhance quality and clinical outcomes for behavioral health patients, and to assure changes could take place in a financially sustainable way.
“Sheppard Pratt Solutions was a partner St. Mary’s could trust to navigate this complex process and help identify the resources needed for success,” said Michael Abbatiello, executive director of Sheppard Pratt Solutions and vice president of behavioral health services at St. Mary’s. “We needed to redevelop day treatment services. At the same time, we wanted to grow interventional services, construct a new unit devoted to geriatric psychiatric services, and expand community outreach and education efforts.”
Significant improvements are already occurring because of the partnership, including a decrease in patient length of stay. New collaborative care systems are in the planning phase and will work in connection with the healthcare system’s primary care network. And work is in progress for the hospital’s new geriatric psychiatric unit.
No two Solutions partners are the same, and Merz says that customization is key when it comes to how the team configures both consulting and management-based partnerships with hospitals and healthcare systems. Some clients require strategic plans and road maps for service line development and growth. Others need support when it comes to service line management—from optimizing leadership and boosting productivity to assuring regulatory compliance, improving quality and performance measures, minimizing barriers to care, increasing access to care, or stabilizing financials.
A steady pace of repeat business, expanded consultation agreements, and the transition to contractual partnerships has meant Sheppard Pratt Solutions has grown exponentially. Since its launch, Merz has continued to expand his core management team. And the need to recruit administrative and clinical experts to serve as site leaders, as additional healthcare system and hospital clients come on board, has been constant.
“We are relentless in our commitment to serving as valuable, quality-based partners for other healthcare systems that need our help,” said Merz. “The work we do is so important and allows us to teach others the best of what Sheppard Pratt offers, while creating access to high-quality services that impact communities in Maryland and beyond. This is why we are continuously asked to do more.”
“The Sheppard Pratt name and brand speaks for itself,” said Shrum. “Organizationally, Sheppard Pratt was a match for us.” Abbatiello expressed similar sentiments, reflecting on the initiation of the contract with St. Mary’s, “All it took was one site visit to the hospital system, and our team knew that Sheppard Pratt was the answer for us.”
Sheppard Pratt Solutions was a partner St. Mary's could trust to navigate this complex process and help identify the resources needed for success.
Opening the "Front Door" to Critical Care
“When it comes to accessing care, people are often encountering a revolving door—one where they get stuck, or there isn’t availability,” said Deepak Prabhakar, MD, MPH, chief of medical staff and medical director of outpatient services at Sheppard Pratt.
At Sheppard Pratt, there isn’t one way into the health system. Sheppard Pratt’s “front door” can look different for each person, depending on their circumstances. Whether you’re experiencing a crisis or seeking long-term support, you can access crucial programs and services at Sheppard Pratt when and where you need it—in the community, through our Solutions’ partner hospitals, or through Sheppard Pratt’s main entrance. How each patient arrives at that front door may vary widely, but the quality of services they receive remains at the forefront of the field. Sheppard Pratt has thought intentionally and strategically about the ways patients might seek care, removing barriers, renovating physical spaces, and streamlining processes to meet the significantly increasing demand for mental healthcare across the country.
“The proverbial front door to Sheppard Pratt looks very different now than it did a few years back,” said Harsh K. Trivedi, MD, MBA, president and chief executive officer. “The COVID-19 pandemic forced healthcare providers to rethink how they interact with and connect with one another and patients. Here at Sheppard Pratt, we have introduced novel approaches that have transformed the way we build and deliver critical mental healthcare services.”
Over time, Sheppard Pratt has grown both physically— with the opening of new, state-of-the-art inpatient and outpatient locations—as well as virtually, with the expansion of telehealth and call center services to create a front door to care that offers increased access for the community.
“Connectivity is so valuable as we put systems in place to eliminate barriers to mental health services and streamline the process of care for our patients,” said Dr. Prabhakar. “The key is getting each patient to the right provider, within the right service area, based on their specialized and unique needs. What sets Sheppard Pratt apart is that we have put an infrastructure in place that allows us to do in a few hours or even a few minutes what it might take days or even weeks to accomplish elsewhere.”
In the past year, Sheppard Pratt has introduced or expanded several key programs and services, all with the focus on making our front door more accessible, more convenient, and more outcomes-focused for the people and their families who entrust us with their care.
A Redesigned Space
The COVID-19 pandemic exacerbated the existing need for mental healthcare services across the nation, driving more patients to emergency departments that are unable to accommodate the increased need. In spring 2023, Sheppard Pratt unveiled its new Admissions, Psychiatric Urgent Care, and main entrance lobby area on its Towson campus to help address the increased demand. This new space serves as the actual front door to the Towson hospital. Psychiatric Urgent Care is the “go-to” place for people who know they need help but don’t know where to start. Here, a licensed clinician conducts an assessment and then makes a recommendation on the type and level of care the person needs. The space was renovated to increase capacity of the Psychiatric Urgent Care by relocating the check-in and waiting area directly next to Admissions, with a single shared team to handle intake. Not only does this provide more space, including additional consultation and exam rooms, but also a quicker and smoother transition to the appropriate ongoing care.
“Our Psychiatric Urgent Care is set up to cater to the needs of people experiencing psychiatric issues, and as it is colocated with our admissions process, patients have greater access to the nearly 400 inpatient beds on any given day. We can transition someone in crisis from an outpatient setting to an acute care setting efficiently and safely,” said Dr. Prabhakar.
“Our data shows that only a third of our urgent care patients require inpatient care. By identifying non-hospital services, we are substantially reducing emergency room visits and prolonged emergency department stays by helping people access care more directly,” said Lynn Stefanowicz, MA, LCSW, chief of access at Sheppard Pratt.
The model of care has also shifted in utilizing collaborative telehealth between the two Psychiatric Urgent Care locations (in Towson as well as the Baltimore/Washington Campus, which opened in June 2021), depending on which location has greater demand that day. On days when one is overflowing with patients and the other is not quite as busy, telehealth providers are ready and available to lessen wait times. Providers from both locations can virtually consult with patients who are physically on-site at another location, which allows patients to connect to care right away.
“We want to do everything we can to provide urgent care, quickly,” said Stefanowicz. “It’s an alternative approach, and we are seeing that many patients appreciate it. It’s a personal choice, but many choose to see a provider immediately, virtually, as opposed to waiting.”
In 2022, an average of 720 patients presented per month in Sheppard Pratt’s Psychiatric Urgent Care locations, combined between the Towson and Baltimore/Washington Campus locations. Between January and March of 2023, that collective average rose to 957 evaluations per month.
Introduction of Sheppard Pratt Admissions Ambulette
As hospital emergency departments (EDs) are experiencing an increase in patients in mental health crisis, facilitating a transfer to another hospital can be a cumbersome, difficult, and sometimes even impossible task for ED doctors and nurses. In tandem, patients often have no choice but to sit and wait, thus experiencing critical delays in getting the care they desperately need. In 2023, the Sheppard Pratt Admissions Ambulette was introduced, offering a solution that has benefited both providers and patients.
“Emergency department providers do a great job, but their focus is not psychiatric care, nor are they typically trained to respond to a psychiatric crisis,” said Dr. Prabhakar. “Sheppard Pratt formalized a transportation service to move patients to our hospital campus for admission and immediate placement into an inpatient bed that was made to care for them.”
The Admissions Ambulette is facilitated in partnership with hospital emergency department teams located within 25 miles of Sheppard Pratt’s Towson and Baltimore/Washington hospital campuses.
“We reach out to the local hospitals every day to make connections and confirm if there are any patients boarded in the ED who may benefit from our ambulette service,” said Stefanowicz. “Being proactive helps us prepare for who is coming in and allows us to start care quicker for patients who need us the most.”
What sets Sheppard Pratt apart is that we have put an infrastructure in place that allows us to do in a few hours or even a few minutes what it might take days or even weeks to accomplish elsewhere.
Meeting People Where They Are Through Mobile Crisis Services
In Frederick, Sheppard Pratt’s Mobile Crisis Services have taken a unique and collaborative approach to physically bring crisis services to people in need, regardless of where they are. Law enforcement, fire and rescue, and Sheppard Pratt mental health professionals work collaboratively to de-escalate crisis situations, put safety measures in place, stabilize patients, and then connect them to programs, services, and other community-based resources. In the city of Frederick, this multidisciplinary approach goes one step further with the use of a Crisis Response Team, which travels wherever it is needed to address crises and de-escalate situations. The pilot, which launched in July 2021, has expanded to eight hours a day, five days a week and has responded to nearly 300 calls in the first four months of the year.
“Addressing crises with this approach ensures individuals receive support for their mental health as well as safety. We have a goal to resolve the majority of the situations we respond to at the scene,” said Willa Naegele, LMSW, program director for Mobile Crisis Services at Sheppard Pratt.
Recently, Sheppard Pratt and the sheriff’s office worked together to launch a new Mobile Response and Stabilization Program, providing up to eight weeks of continuous service to resolve crisis situations for families with children.
“We have seen a huge increase in the number of kids who are experiencing crisis, so having a team that is specially trained to respond in situations that involve children and adolescents has been key,” said Naegele. “The demand for our services is increasing as more people learn about who we are, what we do, and how we can help.”
Using Technology to Transform the Way We Deliver Care
It’s no secret that the world we live in today is a high-tech one. In the healthcare environment, technological tools can be used to streamline and document patient care, expedite communication among providers and patients, and optimize clinical operations. Sheppard Pratt is relying on technology in especially innovative ways, with a focus on collecting outcomes data and feedback from patients to transform the way mental healthcare services are offered, delivered, and improved over time.
“We have been leveraging PROMs, or Patient Reported Outcome Measures, for a while, but we recently put new systems in place to further embed the tool across our entire healthcare system so that we can better understand and learn from the patient care journey,” said Todd Peters, MD, vice president and chief medical officer and chief medical information officer at Sheppard Pratt. “We are engaging with our patients in new ways, and the information they provide allows us to deliver better care for that individual and benchmark against ourselves to improve care in every service.”
Sheppard Pratt’s PROMs platform was built and developed using an open-source technology stack, which allows for connection with the broader technology community. These collaborations help facilitate the addition of new features, the immediate execution of system improvements, and expedited problem solving. The format is flexible, scalable, and compatible with other existing Sheppard Pratt technologies, allowing for seamless integration and easy access to information that can improve how patient care is delivered.
“PROMs provides a direct assessment of patient perspective and collects information that cannot always be captured through clinical measures alone,” said Matthew Payne, director of data management, analytics, and reporting (DMAR) at Sheppard Pratt. “By systematically measuring and monitoring PROMs, we can track what happens with our patients in terms of their symptoms, functionality, and quality of life. This information empowers our clinicians to make informed treatment decisions, facilitate personalized patient interactions, and engage in shared decision- making with patients and their families.”
PROMs is part of a series of technical tools built into Sheppard Pratt’s DMAR Hub. Collectively, these tools provide organizational leaders and clinical providers with important operational data, quality indicators, and performance data that puts the spotlight on developing the right solutions.
When patients provide feedback, they positively impact their own care and help improve care for others. Trends are in real time and can be reviewed immediately to inform treatment team decisions. Leaders can then talk through best practices and understand how to improve, as well as use the data to highlight the people and processes that are making strides.
“Everything we do is about helping our community make informed decisions,” said Payne. “Technology helps us validate our operations, assures our clinical goals are on track, and provides standardized methodologies for supporting patient progress.”
Ryan Gruver, director of operational excellence at Sheppard Pratt, works to identify opportunities for operational improvement aligned with Sheppard Pratt’s strategic plan. He leverages data and information from the DMAR Hub for real-time insights on how the organization is performing in terms of efficiency, productivity, quality, value, cost containment, patient experience, and patient outcomes. Key takeaways are actively driving transformation across Sheppard Pratt’s hospitals, schools, and community-based programs.
“We study the data to identify trends, which then informs critical programmatic decisions,” said Gruver. “We gathered information that guided the redesign of the patient intake process. As referrals come in from local emergency rooms, our new processes reduce the gap in time between when a patient is discharged from a bed and the next patient can get in. We have optimized how we route calls as they come into our call center, to assure patients are directed to the right person for immediate triage and then to the right clinical provider for long-term care. The positive impact on care coordination, and therefore patient experience, has been significant.”
As many healthcare institutions face a national nursing shortage, Sheppard Pratt has found creative solutions leveraging technology and communication across the health system to meet patient needs. “We have platforms that monitor many aspects of patient care and staff experiences on our units,” Gruver said. “We use our human resources information system to understand staffing gaps in real time. We can visualize staffing to census ratios, adjust for acuity, and then allocate our staff to the places they are most needed. We are also continuously brainstorming ways to streamline provider and nursing documentation, which provides caregivers more time to do what they do best—care for patients.”
“The intention of using these technologies is to take a field that is very subjective and make it objective,” Dr. Peters said. “We can use our patients’ own words and their measurable improvement over time to provide better care and better outcomes for everyone.”
Changing Lives Through Innovative Community Partnerships
“Sheppard Pratt is not just a hospital; it is a system of care in the community,” said Jeff Richardson, LCSW, MBA, vice president and chief operating officer for Sheppard Pratt’s Community Services programs. “We use partnerships to help people stay successful and in their communities.”
Through the establishment of innovative partnerships with healthcare providers, community-based nonprofits, and local businesses, Sheppard Pratt is helping people access the resources they need. To improve quality of life for the individuals and families in its care, Sheppard Pratt is not only investing in new facilities, renowned clinical experts, and state-of-the-art technologies, but also comprehensive, community-based services that meet people where they are. The concept is collective impact.
Here, we spotlight a few ways we are partnering in our communities that are making a life-changing difference for the people Sheppard Pratt is committed to serving—from colocating care providers to successfully transitioning students with special needs into the workforce.
The Establishment of a Community Wellness Hub
In late 2022, the Sheppard Pratt Community Wellness Hub opened to serve residents of northern Montgomery County. It unites a collection of community partners together under one roof to address health, social, and workforce service needs in a nonprofit service desert in upper Montgomery County, which was experiencing fast population growth as well as increasing socioeconomic challenges.
“Connectivity is key,” Richardson said. “Our experience has taught us that people often need more than just one type of service, and the Wellness Hub is a one-stop shop where they can turn for various resources they need to thrive.”
Food and housing assistance, educational support, childcare resources, legal services, workforce development programs, crisis and emergency services, and healthcare—including mental healthcare, vision, and dental services—are integrated into the partnership model. Sheppard Pratt’s Thriving Germantown Program is housed at the Wellness Hub, offering multigenerational, multitiered case management and care coordination for children and their families living in poverty. Also on-site is the Sheppard Pratt School and Community Youth Services Program. This program provides youth and family therapy services, crisis intervention services, support groups, therapeutic recreational services, skill-building programs, and other mental health and wellness-focused services in line with demonstrated community need.
“It is important that people know Sheppard Pratt is vested in creating a system of care that is accessible in our communities, too,” said Richardson. “The Wellness Hub is one example that models that commitment. It demonstrates how Sheppard Pratt has taken the lead in bringing people together from various organizations to create a model of care that really benefits people, tends to their needs, and provides valuable, accessible resources.”
The Sheppard Pratt Wellness Hub is a bridge that links families to resources. Other partners offering services include EveryMind; American Diversity Group; Care for Your Health; Casa Ruben Foundation; Feed the Fridge; Healthcare Initiative Foundation; National Capital Presbytery: Germantown Global Connection, Creekside Church, and Earthen Hands; The UpCounty Hub; and Upper Montgomery Assistance Network.
“As partners, we are committed to creating impact in Montgomery County that shows positive, measurable outcomes,” said Richardson. “The Wellness Hub is allowing each partner to make connections and do things as part of a collective impact program. Our communities need more collaborative approaches like this to help people and families achieve mental wellness and access to much-needed services to support them today and in the future.”
Sheppard Pratt is not just a hospital; it is a system of care in the community. We use partnerships to help people stay successful and in their communities.
Preparing Young Adults for Workforce Opportunities
Over the years, Sheppard Pratt Schools have focused on creating a positive and supportive educational environment for children with special needs to learn, grow, and thrive. As students approach adulthood, begin exploring career interests, and face the end of school-based healthcare services, Sheppard Pratt helps them prepare to be successful once they graduate. Sheppard Pratt Schools’ comprehensive vocational training programs, coupled with partnerships with local businesses, create new pathways for young people to gain valuable experience in and exposure to the workforce to continue to lead successful lives.
“It is so important that we equip our students with connections and skills proactively, so they can go out into world and be thriving members of the community after graduation,” said Claire Cohen, LCSW-C, regional director of Sheppard Pratt Schools.
The value of this work is made clear through stories of former students who have found fulfilling employment opportunities, and in some cases, even entrepreneurial opportunities. One former student who discovered a passion for auto mechanics during his time at Sheppard Pratt School in Rockville went on to attend a trade school and is now headed into his third year of gainful employment at a local automotive shop. Other former students have taken the skills they practiced in these vocational programs and turned them into full-time work at the same local restaurants, recycling centers, and retail stores where they interned.
“Through our partnerships with local businesses, students from Sheppard Pratt Schools have opportunities to build key core life skills—from cleaning, stocking and restocking, to knowing how to greet and communicate with customers, use money, use public transportation systems, and problem solve,” said Cohen. “There is so much value in putting our students into these environments, where they can learn these important skills and gain independence and confidence, while their support systems are still in place.”
Project SEARCH is another program that helps young people with special needs find and secure meaningful employment so they can grow and thrive personally, gain independence, and be active members of the community. The program is facilitated through a partnership between Sheppard Pratt, Anne Arundel County Public Schools, and The Arc of Central Chesapeake Region. It opens doors for young adults to gain hands-on work experience through internships at places like the BWI Hilton Hotel and Anne Arundel Medical Center.
“Project SEARCH allows us to find promising opportunities for our special education students in line with their strengths and interests, guide them as they become immersed in the workforce, and support them as they get acclimated in their new roles,” said Kathy Flannery, MEd, regional director of Sheppard Pratt Schools. “Through these experiences, our students learn how to hold a job, build new skills, and begin to make the transition from being a student to a productive adult.”
At the BWI Hilton Hotel, Project SEARCH interns have opportunities to work in the kitchen and laundry facilities, as well as support special events that are held in on-site conference rooms. At Anne Arundel Medical Center, interns have worked in human resources, marketing, the cafeteria, on research teams, and in some clinical care environments.
“The workforce is more diverse today than ever before, and Project SEARCH is designed to prepare people for success through a combination of classroom instruction, career exploration processes, training, and practical experience,” said Flannery. “We are grateful for our partners and their commitment to supporting students with neurodiverse needs, who otherwise may have difficulty finding these kinds of opportunities.”
Care & Services: Here and Now
Over the past few years, the need for behavioral healthcare has grown at an explosive rate. We responded to that need by expanding our programming and access to it. The future that we have been building toward is here, and our ever-growing network of more than 160 high-quality programs and services will continue to evolve as we lead the way in responding to the growing behavioral health needs in Maryland and beyond.

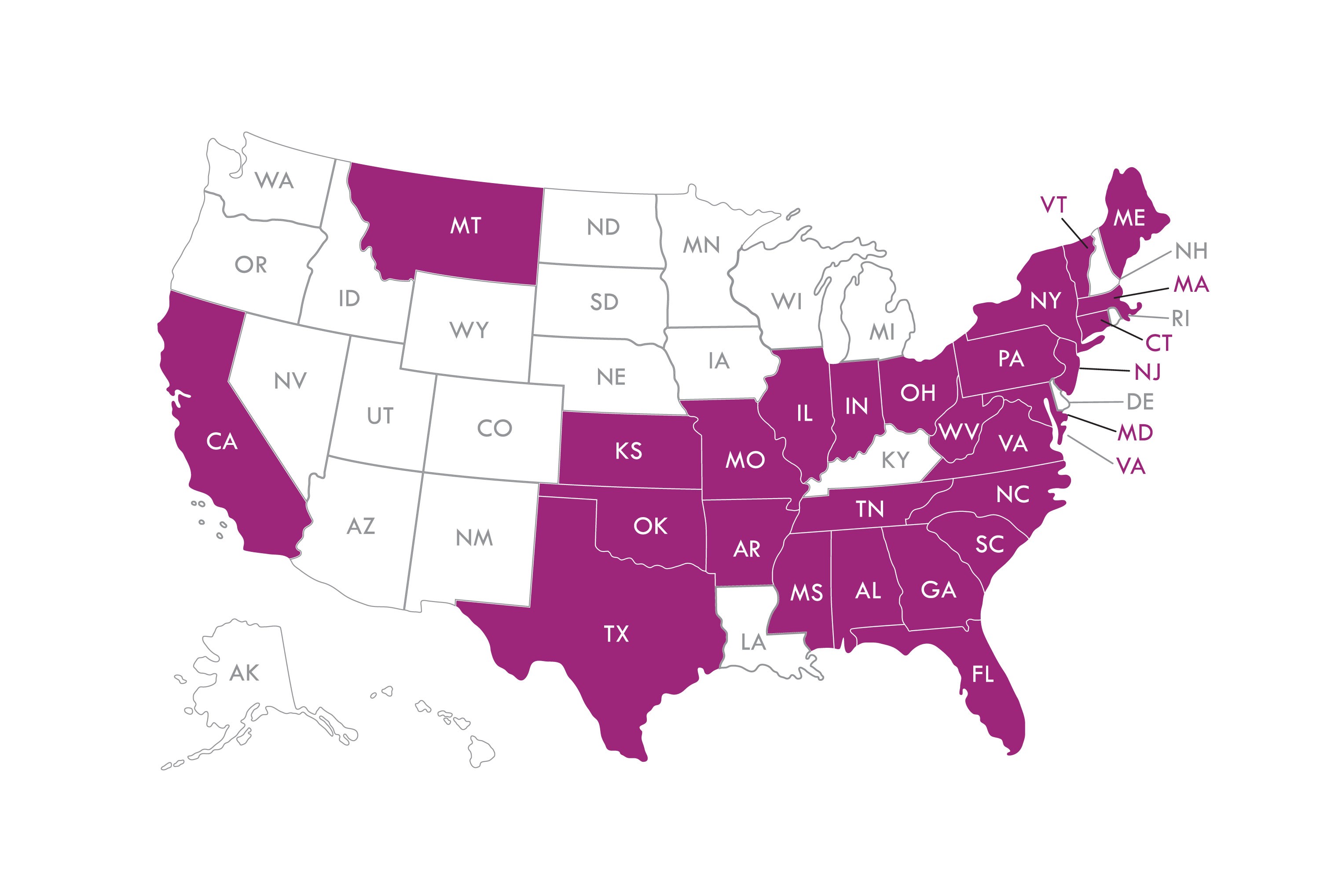
Sheppard Pratt Solutions partners with hospitals and health systems throughout the country.
Statistics & Financial Highlights
Net Revenues (in millions of dollars), Sheppard Pratt
- FY '22: $400.5
- FY '23: $457.6
Sheppard Pratt Statistics FY '23
- Inpatient days: 110,919
- Educational days: 111,622
By the Numbers
Approximately 11,000 visits to our Psychiatric Urgent Care and Mobile Crisis Programs
More than 50,000 outreaches for services through calls, website inquiries, and our chatbot, Hope
More than 15,000 youth served across all programs and services
More than 20,000 Patient Reported Outcomes completed to improve patient care
Nearly 80,000 individuals served in our programs and through our partnerships with hospitals and health systems across the country
2023 Leadership & Board of Trustees
Officers and Executive Staff
Harsh K. Trivedi, MD, MBA
President and Chief Executive Officer
Kelly Savoca, CPA, MBA
Senior Vice President and Chief Financial Officer
Jennifer Weiss Wilkerson, MHSA, FACHE
Senior Vice President and Chief Strategy Officer
Stacey Garnett, RN, MSN, FACHE
Vice President and Chief Nursing Officer
Gregory Gattman, FACHE
Vice President and Chief Operating Officer, Hospitals
Jeffrey Grossi, JD
Chief of Government Relations
Thomas D. Hess, MBA, MEd
Chief of Staff, and Interim Chief of Schools
Stephen M. Merz, FACHE
Chief Operating Officer, Solutions
Todd Peters, MD
Vice President and Chief Medical Officer and Chief Medical Information Officer
Donna L. Richardson, MBA
Vice President and Chief Development Officer
Jeff Richardson, LCSW-C, MBA
Vice President and Chief Operating Officer, Community Services
Karen Robertson-Keck SPHR, SHRM-SCP
Vice President, Human Resources
Board of Trustees
Margaret Allen
Kevin M. Benson
Alan Evans
Susan Fenimore
Elizabeth Forbush
Alan Gamse
Philip H. Grantham
William Haugh
Bonita Hearn
Joshua Kakel (Chair)
Norma Peden Killebrew
Martha Kirkland
Alton Knight
Robert Kresslein
Cristin C. Lambros
William Morton
Collin Mothupi (Vice-Chair)
Alfred Singer (Vice-Chair)
Jim Wiederhold
Stephen Judson Williams
A Message from Development
Dear Friends,
Mental healthcare has made significant advances since Moses Sheppard and Enoch Pratt left legacies to create the health system that bears their names. The founders had a forward-thinking vision, and their philanthropy set in motion the beginnings of modern mental healthcare at a time when few such services were available.
Sheppard Pratt continues to be a leader and innovator in mental healthcare. Since our founding in 1853, we have provided patients with an environment where they can receive critical care in comfort—rooms with windows, beautiful grounds, respectful treatment, and a commitment to providing care guided by best practices. While that commitment, and the environment it was built into, still stands, it now includes state-of-the-art inpatient and outpatient programs, cutting-edge research into treatments for persistent depression, and specialized centers to treat people with autism, eating disorders, OCD, anxiety, and more. We have become a thought leader and model for healthcare organizations across the country. Hospital systems and individual mental healthcare providers alike turn to Sheppard Pratt for our unique expertise to help improve and grow their own programs.
Throughout Sheppard Pratt’s history, we have relied on generous donors to fuel our innovative work. While the best clinicians and staff members walk our halls, the resources required to ensure continued excellence depend upon philanthropy.
We owe a deep debt of gratitude to the donors listed in our online report, who have supported Sheppard Pratt throughout the year. Their contributions have improved the lives of countless patients, families, and entire communities. A special thank you to Pedie and Bob Killebrew for their generous support, which enabled the RAND Corporation to conduct an analysis and case study of Sheppard Pratt to understand how our experiences can potentially inform national mental health policy.
The needs of our communities are great, and more is required. The forward-thinking vision of our founders, and the future we have been working toward, is needed now more than ever. Initiatives are already underway to meet urgent mental health needs, especially for our nation’s youth. We carefully evaluate every program we offer and expand those that are having the greatest impact. We continue to work with healthcare policymakers and insurance companies to ensure that mental illness is treated with the same importance as physical illness. The future is now. We must act to make a difference for the countless individuals and communities who rely on us.
In the five years since I arrived at Sheppard Pratt, I have never been more enthusiastic about the way we are evolving and expanding to serve all those in need of our care and services. From children to older adults, for veterans, families, people struggling with substance use disorders, and for the most vulnerable in society—Sheppard Pratt has created a continuum of care that does it all. The future we have been preparing for is now. With you, we have built a strong foundation, and with your support, we can continue to fulfill our mission: to lead, to care, to respect, and to meed the need—no matter how great.
Sincerely,
Donna L. Richardson
Vice President and Chief Development Officer
Sheppard Pratt surpassed its initial $100 million "Now More Than Ever" campaign goal to expand mental health programs and services. This funding supported:
- Establishing the Institute for Advanced Diagnostics and Therapeutics
- Establishing the Center for Autism
- Expanding capacity of our walk-in urgent mental healthcare services
- Rewarding the talents of the top teachers at our schools
- Creating an employment training center for veterans
Our new campaign sets a bold vision to transform youth mental health. Investing in the care of a child at an early age will help them live better, more fulfilling lives. There has never been a more critical time. Our donors and partners play an important role in the future of our youth.
Please join us on this journey.
Our Donors & Partners
Our donors and partners play an important role in helping us lead the way. With your support, we will continue to meet the unmet mental health needs of our communities. Annual Giving Circle of Friends recognizes new pledges and gifts of $100 and above received between July 1, 2022 and June 30, 2023.
$1 million and above
Kim and James C. Davis
State of Maryland
Substance Abuse and Mental Health Services Administration
U.S. Department of Labor
U.S. Department of Veterans Affairs
$250,000 and above
Montgomery Coalition for Adult English Literacy
Maryland Department of Transportation
Truist Foundation
Women's Hospital Foundation
$100,000 and above
Bender Foundation
Cordish Family Foundation
Greater Washington Community Foundation
Horizon Foundation
Maryland Department of Health
$50,000 and above
Behavioral Health System Baltimore
Morris and Gwendolyn Cafritz Foundation
Frederick County Public Schools
Mr. and Mrs. Robert S. Killebrew
Nancy B. Paternotte and William L. Paternotte
$10,000 and above
Margaret Allen and Philip Perkins
Anne Arundel County Department of Health
Benchmark Construction Company
Bunting Family Foundation
Mary Catherine Bunting
H. Bruce Fenwick
Susan and Andrew H. Friedman
Healthcare Initiative Foundation
Elayne Hurwitz
Interfaith Works
Duke and Jane Kassolis
Emily Catherine Leichter
Leonard Paper Company
Gary Mann
Wilson Mann
Maryland State Department of Education
Mead Family Foundation
National Council on Alcoholism and Drug Dependence
John A. Nesbitt, III, MD
PNC Foundation
RxBenefits
Estate of Carolyn W. Sanger
Kathy and Sandy Shapiro
Gail and Stephen Shawe
Gordon and Jean Wells
$5,000 and above
Mr. and Mrs. Edward H. Berge, Jr.
Samuel M. Dell, III
General Healthcare Resources
Philip H. Grantham
Joshua Kakel
Cristin C. Lambros and Matt Levinger
Kenneth and Carol Lew
Marshall Craft Associates
Drew Pardoll
PMM Companies
Joel Ranadive
The Nora Roberts Foundation
Schneider Electric Buildings Critical Systems
$2,500 and above
Allegeant
Allied Telephone and Data Corp.
Beth Babikow
Kevin M. Benson
Eric Case
Diane and Robert Gingell
Hall, Render, Killian, Heath & Lyman
Thomas D. Hess
Andrew and Sandy Levy
Mr. and Mrs. Douglas P. McDaniel
Elizabeth and John Miklos
Karen Robertson-Keck
Skyline Technology Solutions
Whole Foods
$1,000 and above
David and Bonnie Allan
David and Deborah Astrove
Amy Bachelder
Baltimore County Employees Federal Credit Union
Bob Davidson Ford
Richard Bullen
S. Winfield Cain
The Campbell Foundation
Centric Business Systems
Mary Lou and Leo Clagett
Christine and John Dinwoodie
District Veterans Contracting
Alan W. Evans
Susan Fenimore
Elizabeth R. Forbush
Laura L. Gamble and Rob W. Gillison
Barbara and Alan Gamse
David Guernsey
Daniel K. Hayes
Elaine B. Johnson
Alton Knight
Dr. and Mrs. Stuart R. Lessin
Kim and Keith W. Lewis
Magnus Chess Academy
Wilma Maye-Eady
Brook and Donna Morris
Collin Mothupi
Lisa Mutschler
Paul Norman
Glynn I. Owens
The PepsiCo Foundation
Michael Phillips
Marie C. Rector
Rogers-Wilbur Foundation
Rosedale Federal Savings and Loan Association
Rossmoor Women's Club
St John's Episcopal Church Norwood Parish
St. Peter's Catholic Church
Carol Sandler
Kelly Savoca
Nancy Schiffer and Goldwin Smith
Jacob S. Shapiro Foundation, Jane and Stanley Rodbell, James R. Shapiro
Richard L. and Annabelle Sher
Alfred and Lisa Singer
Claire M. Smith
Mr. and Mrs. John W. Steele, III
Dr. and Mrs. Harsh K. Trivedi
Edward and Margaret Trojan
Joanna and Alan Wallenstein
Robert Wieder
James Wiederhold
Jennifer Wilkerson
Gay and Jud Williams
Mr. and Mrs. Alfred A. Windesheim
$500 and above
All-Shred
Susan Bellamy
Donna and Ronald Blanck
Donald and Janet Boardman
Susan and Robert L. Bodansky
Bruce S. Campbell, III
Marina Cecchini
Comm-Tronics
Abbie L. Cornblatt
Gerrit Fitch
Mitzi Francis
Frederick Foot & Ankle
The Frederick Keys
Frederick News-Post
Greg Gattman
Nancy Gieser
David Goode
William L. Haugh, Jr.
Bonnie and Biff Hearn
Frederic F. Hinze
Steve Kaelber
Martha Kirkland
Robert Kresslein
Kirill Lokshin
Diane Maistros
Maryland Office Interiors
Parsons Corporation
Todd Peters, MD
Mr. and Mrs. Arnold H. Quint
Jodi Reedy
Albert and Kathy Schiffer
LaTonya D. Shedrick
Laura Simmons-Smith
Shelley and Kevin Summerville
Susan and Andrew Vanhorn
Daniel Weissbarth
$100 and above
Acropolis Construction
Patricia F. Adams
Jason Addison, MD
Joanne Aellen
Amazon Smile Foundation
Diane and Owen Ambur
Susan and Mark Andrews
Patricia A. Arkuszeski
Andrea and Michael L. Ault
William J. Ault
Jim and Judy Bailey
Anne D. Bailliere
Bedford Road Volunteer Fire Department
Karen and George W. Benson, III
Shannon Bergeron
Shekya C. Berkley
John Biggs
Anna and Dennis Bivens
The Blackbaud Giving Fund
Karyn Blad
Martha Blakeney
James D. Blum
David Bolick
Kimberly and Thomas Bonvissuto
Felicia Bracey
Allison Brill and Peter Kwiterovich
Michele L. Brill
Charletha T. Brown
Jacquelyn F. Tate and Douglas M. Burch
Catherine Burroughs
Ryan Burton
Caroline Perlman Cahn
Curtis Campbell
Capital Group Companies Charitable Foundation
Jeanne Carfine
Don and Julia Carlson
Catherine and Fred A. Cecere
Pamela Chambliss
Emma Collie
Jennifer Crawford
Susan M. Cromwell
Merilee Cummings
Ellen Curry
Da Capo LLC
Glendoris Dantoni
DASA-PPR
Christine Dingivan
Laurie DiRocco
David Drake
Gerald Eichner
Carolyn Ericson
MD Farrell Plumbing
Kristi Fleming
Folstad McUmber Charitable Fund
Maria Fontaine and David Brlansky
Peter H. Gambrill
Chris and Ruth Gammon
Jorge and Caren Garayta
Stacey Garnett
Ellen Gelles and Steve Ricanati
Nancy S. Grasmick
Peter Greco
Laurie Greene
Jane and David Greene
Sarah E. Gunning-Schell
Mark J. Hajjar
Haines Hotel Services Group
James M. Hannan
Lindsay Hardesty
Barbara Harms
Fred and Linda Hasecke
Christopher Hertz
Robert Hickey
Guy and Susan Hicks
Daniel and Gina Hirschhorn
Karla Hoffman
Keisha Hogan
Trish Hollar
Susan Holloway
Brian Hoover
Mr. and Mrs. John R. Jackson
Leah and Donald Jordan
Miriam Katowitz and Arthur J. Radin
Kimberly Kavanagh
Emily G. Kishter
George and Mary Koch
George Korengold
Gerrit Kuechle
Ryan Lang
Nancy Langis
Tina Lauber
Jimmy Li
Valerie Lovelist
Lawrence Lubetsky
Dorothy B. Lyles and Amy E. Dunsmore
Amy Macht
Wayne Maddox
Rachel Matera
Mervyn Matteson
Kimberly McCabe
Susan McCormick
Prasanna Menta
Amy Meyerl
Montgomery County Alumnae Chapter of Delta Sigma Theta
Ken and Betsy Morrow
Magen Morse
William A. Morton, Jr.
Angela Myers
Sarah Norman
Ann Ortega
Thomas Owen
Padonia International Elementary
Janet Parrish
Donald and Maria Pazour
Theresa Peddicord
Matt Peeling
Wendy and Charles Phillips
Gail Phillips
Brian Piccolo
Cristen Piontek
Shari Price
Danielle Queen
Ann H. Reilly
Robert and Maura Reiver
Donna L. Richardson
Nicholas Riley
Patrick J. Ryan
Doug Ryczko
M. C. Savage
Jason A. Scaroni
Robert and Marilyn Schaftel
Diane Schechter
John Shirk
Rosanne K. Silberman
Nathan I. Silver
Ted and Lisa Sjurseth
Patrick Slattery
Nancy Sneed
Lynn Stefanowicz
Mary and Donald Summerville
Steve Surdez
Jaclyn Svincek
Amy Swam
Yasir Tarabichi
Erin S. Thompson
Jean and William W. Thompson
Tribe Cycle LLC
Tara Watts
Eileen Weinstock
Kelly and David Wenner
Frances and Frederick A. Wenner
Brett and Kathy Widenhouse
John Wieseman
Katie Wilburn
James Willard
Cynthia Williams
Richard Williams
Joan Wisner-Carlson and Robert W. Wisner-Carlson, MD
Danielle K. Yearick
Honor & Memorial Gifts
The people listed below were honored with gifts of $100 or more between July 1, 2022 and June 30, 2023.
In memory of Harriet E. Andrews
Susan and Mark Andrews
In memory of Ray Ault
Andrea and Michael L. Ault
William J. Ault
Donna and Ronald A. Blanck
Catherine and Fred A. Cecere
Amy and Timothy B. Dunsmore
Jorge and Caren Garayta
Julie and Benjamin R. Kerth
Dorothy B. Lyles and Amy E. Dunsmore
Lynn McCall
Michael A. McCall
Elizabeth and Lee McMillan
Mary and Donald C. Summerville
Shelley and Kevin Summerville
Jean and William W. Thompson
Susan and Andrew Vanhorn
In memory of Matthew M. Blacker
Bedford Road Volunteer Fire Department
In memory of Brenda M. Callbeck
Nancy S. Grasmick
In honor of Mark F. Carter
Leilani Tydingco-Amarante
In memory of Anna M. Dasbach
Emma Collie
In memory of Nancy Diener
Brett and Kathy Widenhouse
In memory of Stacy N. Dorsch
Karen and George W. Benson, III
In memory of Andrew Drake
Donna L. Richardson
In memory of Michael Francis K. Hammaker
Nathan I. Silver
In memory of James Howe
Paul Norman
In memory of Charles Kaelber, MD
Joanne Aellen
All Smiles Bethesda
Jim and Judy Bailey
Christina Bauer
Bernita Beck
Brian and Dian Belanger
Catherine Burroughs
Jane Caputo
Allan Carlson
Don and Julia Carlson
Ellen Curry
Gerrit Fitch
Alan and Arline Fraser
Ellen Gelles and Steve Ricanati
Peter Greco
Joan Guberman
Barbara Harms
Fred and Linda Hasecke
Steve Kaelber
Ernest and Brenda Kessler
Allan and Irene Kirkpatrick
Gerrit Kuechle
Martha Kuhlman
Dennis Luther
Mervyn Matteson
Steve and Kay Mitchell
Ann Ortega
Nicholas Riley
Chuck and Judy Sturtz
Yasir Tarabichi
Washington Commanders Marching Band
Dorothy Welsh
John Wieseman
In memory of Jackie Kleiman
Tara Watts
In memory of Karl I. Lanocha
Mind Bend Mental Health
Bruce S. Rosenblum, MD
In honor of McKennah J. Lauber
Tina Lauber
In memory of Kathy MacNeil
Nancy Sneed
In memory of James Nesbitt
John A. Nesbitt, III, MD
In honor of Padonia International Elementary Families
Padonia International Elementary
In honor of Carolyn Paterson
Robert Wieder
In honor of Bonnie E. Phillips
Gail Phillips
In honor of Kara Pokras
Diane and Owen Ambur
Susan Levine
In honor of Donna L. Richardson
Julie S. Marshall
In memory of Carolyn W. Sanger
Jane and David S. Greene
In honor of Deb Schechter
Diane Schechter
In honor of Steven S. Sharfstein, MD
Carolyn Ericson
Mr. and Mrs. Arnold H. Quint
In honor of Sheppard Pratt Human Resources Department
Patricia A. Arkuszeski
In memory of Michael I. Smith
Capt. Amelia and Grant Howerton
Albert and Kathy Schiffer
Nancy Schiffer and Goldwin Smith
In memory of Maxwell A. Tagg
Elizabeth Ash-Conklin
Nathan and Gwynne Benfell
Martha Blakeney
Merilee Cummings
Carolyn Davis
Chris and Ruth Gammon
Robert Hickey
Guy and Susan Hicks
Trish Hollar
Shannon Linford
Magness Chess Club
Randa McBride
Kimberly McCabe
Melanie Miller
Magen Morse
Teresa Noel
Victoria Ogus
Ted and Lisa Sjurseth
Nancy Stucki
Rachel Weidenhamer
The Weidenhamer Family
Adam Weissbarth
Daniel Weissbarth
In memory of Nancy Thayer
Nancy Sneed
In memory of Casey M. Toomey
Randall and Lisa Torrence
Roseanne Fontaine
In memory of Ian Toomey
Maria Fontaine and David Brlansky
Rachel Matera
In memory of Aiden Tremaine
Peter H. Gambrill
In honor of Harsh K. Trivedi, MD, MBA
Eileen Weinstock
In memory of Jan B. West
Anonymous
In memory of Ronnie P. Wieder
Robert Wieder
In honor of Gay Williams
Jud Williams
In honor of Young Adult Inpatient Unit
Laura Simmons-Smith
1853 Society
The 1853 Society recognizes individuals who have made the gift of a lifetime by including Sheppard Pratt in their estate plans.
Anonymous (4)
Emile A. Bendit, MD
Mikki Buchness
John and Sue Carnell
Lois G. Carr
Patricia Castillo
Evelyn Feldman
Elizabeth R. Forbush
Anne Dee Goldin
Louise A. Hager
Joan S. Harris
Charles E. Herget, Jr.
H. Thomas Howell
Nancy Kaelber
Mildred Kern
George E. Kostritsky
Peter J. Lagemann
Jane C. Larson
Janet E. Lowman
James and Sonia Maher
Douglas Miller
Lila E. O'Meara
Patricia A. Prugh
Ruth T. Ravenel
Donald R. Ross, MD and Eileen K. Steinberger, MD
Carolyn W. Sanger
Robert and Marilyn Schaftel
Drs. Margaret and Steven Sharfstein
Dr. and Mrs. Edward Sienkilewski
Gordon and Jean Wells
Elise and Dr. Clifford Wheeless
Jud and Gay Williams
Mary Elizabeth Zumstein







